How do people do health in Pakistan? Understanding Health Related Choices and Healthcare Navigation
Ideally, people should be able to embrace health-promoting behaviors and practices and be appropriately informed if they must make life-altering health decisions. Health-related choices that people make daily are critical for recognizing structural shortcomings, targeting particular health-promoting policy interventions, and mapping out people-centered institutional improvements. In Pakistan, along with communicable diseases that continue to represent a significant threat to public health, the burden of non-communicable diseases is also escalating. Addressing these health challenges and targeting structural improvements calls for understanding of the health culture prevailing in communities.
In Pakistan, besides the public and private formal allopathic healthcare systems in place, informal providers practicing allopathy, homeopathy, and eastern medicine are considered to make up a significant portion of the healthcare market. On the consumer side, many socio-cultural, economic and geographical factors contribute to determining health-related choices, healthcare utilization, and navigation. These factors determine when, where and why people seek formal or informal health care. For instant, Khan et al. (2015) found that about 40.7% of the breast cancer patients who delayed seeking allopathic health care first wasted time using alternative medicines. A considerable majority of women with breast cancer in North Pakistan are enduring presentation delays due to their misunderstandings about the disease. Likewise, Mirza et al. 2009, found a significant time gap between identifying developmental issues and seeking medical help in rural Pakistani communities. In Pakistan, even a high level of health literacy doesn’t necessarily translate into a high level of health well-being. The socio-cultural and religious beliefs play an important role in the health-seeking decision of the people (Abdullah & Zakar, 2020). Moreover, there is a dearth of public awareness concerning mental diseases, and treatments related to mental health are widely limited and tabooed (Munawar et al., 2020).
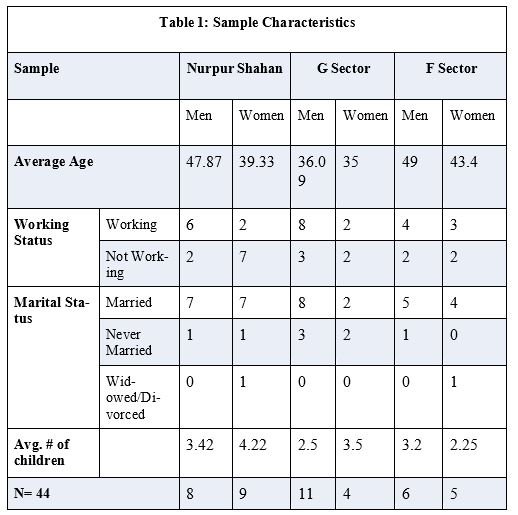
The purpose of this knowledge brief is to understand the lived experience of people about their health; how people take care of their health, when they seek medical help, how they navigate health care systems (formal and/or informal), and how and where do they acquire health information from. We have discussed the each theme in detail below. Table one shows the sample characteristics of our study.
| A note on Methodology We used semi-structured in-depth interviews to acquire data from people currently living in Islamabad for this study. We developed an interview guide to explore the people’s lived experiences on health care maintenance, choices, and navigation. We have collected the data from three different residential areas in Islamabad that roughly present people from different income groups; Nurpur Shahan (a rural locality), G-6, G-9 sectors (middle-income residential areas), and F6, F8 (posh residential areas). A total of 44 interviews were conducted. All interviews were transcribed verbatim. Before the interview, each respondent was asked to read and sign the consent form. After the collection of data, we mined the data for emergent themes. |
Maintaining Health
When asked how you maintain your health on a daily basis, we receive a spectrum of responses from the participants across three residential areas. The respondent of rural area Nurpurshan stressed eating a healthy diet. Not a single respondent was taking any unprescribed dietary supplement. At the same time, the trend of taking unprescribed supplements is quite common among the participants of the G and F sectors. A few respondents from the high-income residential areas mentioned their obsessions with taking the supplement. These include taking supplements for boosting and maintaining calcium, iron, zinc, and multivitamins levels in the body. A few participants mentioned taking the supplement to improve nails, skin, and hair. The respondents from the F sector also mentioned that they prefer to take the imported supplement as they are of high quality.
Delay in Seeking Treatment
A majority of the respondents from all the three residential areas mentioned that they delay treatment and try self-medication first for the diseases they perceive as non-threatening. People take over-the-counter medicine for fever, flu, cough, and seasonal allergies. For most gastrointestinal issues, a majority try home remedies first before seeking formal or informal health care. Most of the participants from all the residents’ areas only see an allopathic practitioner when they perceive the disease as “serious’, “not responding to home treatment,’ or “getting worst over time.” Most of the participants across the residential area mentioned that they usually do not delay seeking treatment if a child in home is sick.
| Allopathic? Hikmat? Homeopathy? A majority of participants in our study seek allopathic treatment if they get sick. Eastern medicine treatment (Hikmat) is usually used as an add-on treatment or treatment for common seasonal viral episodes such as flu and cough. Homeopathy is taken as a serious alternative or parallel treatment along with allopathy. Homeopathic medicine is popular for a range of diseases, including kidney stones, migraine, arthritis, hypo/hyperthyroidism, and Sciatica, to name a few. |
Homeopathy- a Popular Treatment
It is noteworthy that homeopathy is a prevalent alternative/ parallel medical treatment that people go for the diseases they think are not curable or less curable in allopathy. Interestingly, the trend to seek homeopathic treatment is very popular among all participants of the study. A majority of the participants report that homeopathic treatment takes time to cure certain diseases but with no side effects. Furthermore, people believe some specific diseases can only be cured by homeopathic medicine. It is important to mentioned that a majority of participants mentioned that for children they prefer allopathic treatment as allopathic medicine response quickly.
Non-Degree Allopathic Practitioners (NDAPs)
One of the critical findings of the study is that for the participants of the rural residential area, visitation to non-degree allopathic practitioners for acute illness episodes is quite common. These are the partitioners who do not have practicing licenses. They might have worked as an assistant pharmacist, a nurse, or a paramedic in the past. Most of the participants do not know the exact qualifications of NDAPs; they mentioned that they are aware that NDAPs are not doctors but have know-how about allopathic medicine. Study participants mentioned that they prescribe medicine, do small surgeries and have medicine available in case of medical emergencies, which, according to participants, work wonders for them. A very few participants from the middle-income residential area mentioned seeking treatment from these NDAPs. None of the posh residential sector participants mentioned seeking treatment from NDAPs.
| The Magical Injection The participants from the rural residential area mentioned that NDAPs often give patients a shot which works most of the time when patients are in severe pain. It is a famous treatment for the residents, and they request it from NDAPs. According to participants, the injection is suitable for a range of diseases. Sometimes along with injection, NDAPs give an IV to the patient. |
Dis/satisfaction with the Formal Allopathic Healthcare Systems
Participants across all residential areas report a certain level of dissatisfaction with Pakistan’s formal allopathic healthcare system. The dissatisfaction is reported for both public and private health care systems in place. For example, participants from the rural residential area mentioned that the treatment for all diseases is costly. Most of the time, they delay treatment just because they cannot afford it. Pubic hospitals do not have all the medicine. Most of the people in this area were clueless about the Sehat card.
The participants from all the sectors also mentioned cases of medical negligence. They mentioned that private health practitioners lack accountability. However, they charge a fortune to patients. Most people also do not know what to do and where to report in case of medical negligence or mal-practicing. Participants also mentioned that private hospitals make unnecessary bills by doing unnecessary procedures and laboratory tests.
| Private or Public? The participants from the rural community prefer to visit a private health clinic nearby in case of sickness. They only visit public hospitals if they are entitled to get treatment or if the treatment requires many laboratory investigations. The reasons for consulting private partitioners are a shorter distance to the facility, trust in partitioners, time-efficient, and better treatment options. Compared to the participants from the rural community, most participants from the middle-income residential areas visit public health facilities. They prefer public health facilities because of the short distance and inexpensive treatment. However, if needed, they do visit private health practitioners/specialists as well. Almost all the participants from the resident of posh sectors visit private health clinics for treatment. They visit a dedicated specialist for different diseases. |
Health Information
A majority of participants in our study from Nurpur Shahan rely on their social capital for acquiring health information. These include neighbors, friends, and other members of the community. Only one participant mentioned that they see youtube videos to get information about diseases and medicine. Participants also mentioned they see doctors and trust their advice regarding caution and dietary restrictions.
The participants from the middle-income residential areas rely on information that they acquire from health care facilities. Few participants (young ) mentioned googling symptoms and diagnoses before they visited doctors. Acquiring health information from the internet is common among the residents of posh residential areas. The ways how participants acquire health-related information also reflect the tangible and intangible resources available to them. It is no surprise that participants from the posh residential area can afford smartphones and the internet compared to those from low-income rural communities. It may also be due to lifestyle and cultural factors.
Religious Healing
Religious healing as a sole method to solve health issues is not very common but exists primarily for the participants from the rural residential area. However, it is noteworthy that most participants in our study, in one way or another, believe in religious healing by adopting different ways, including but not limited blowing (dam), wearing amulet (taweez), and recitation of specific Quran verses on a daily basis. The use of blowing is common among residents of the rural community. Participants seek such help to cure diseases ranging from infertility to general headaches. Many participants from middle-income and high-income residential areas mentioned that they believe in religious healing for mental health issues such as coping with depression, anxiety, and daily stress. However, not a single participant from the high-income residential area mentioned that they ever used amulet and blowing to get cured physically or mentally.
Key Take-Aways
Several points of concern emerged about health care choices and navigation, and therefore, points of intervention for healthcare policymakers and practitioners.
- Excessive unprescribed supplement taking is common among residents of high-income income areas.
- The majority of participants reports delay in seeking treatment. People only engage with formal healthcare when they perceive disease as “serious,” that is, to most of them, when they will not get better after trial and error of trying various home remedies or by using over-the-counter medicine.
- Homeopathy is a very popular health treatment that people seek compared to or in parallel with allopathy.
- Participants from the rural residential area often visit Non-Degree Allopathic Practitioners for acute illness episodes. The preference for NDAPs is not only because of the availability of these practitioners in the area but also because NDAPs are community insiders. The geographical, social, and cultural proximity plays a major role in why the people trust these practitioners.
- A majority of participants showed dissatisfaction with the allopathic formal health care system in Pakistan. Factors contributing to this dissatisfaction with formal healthcare are medical negligence, behavioral mistreatment of healthcare providers, expensive health care, unhygienic facilities, and malpractice, including making profits by prescribing unnecessary treatments.
- Most participants mentioned seeking religious help to cope with mental health issues without any other medical or counseling intervention. Participants in the rural residential area seek religious healing to cure many diseases, including infertility, kidney stones, and arthritis, to name a few.
References
Abdullah, M., & Zakar, P. D. R. (2020). Health literacy in South Asia: Clarifying the connections between health literacy and wellbeing in Pakistan. South Asian Studies, 34(2).
Khan, M. A., Hanif, S., Iqbal, S., Shahzad, M. F., Shafique, S., & Khan, M. T. (2015). Presentation delay in breast cancer patients and its association with sociodemographic factors in North Pakistan. Chinese Journal of Cancer Research, 27(3), 288.
Mirza, I., Tareen, A., Davidson, L. L., & Rahman, A. (2009). Community management of intellectual disabilities in Pakistan: a mixed methods study. Journal of Intellectual Disability Research, 53(6), 559-570.
Munawar, K., Abdul Khaiyom, J. H., Bokharey, I. Z., Park, M. S. A., & Choudhry, F. R. (2020). A systematic review of mental health literacy in Pakistan. Asia‐Pacific Psychiatry, 12(4), e12408.
Sudhinaraset, M., Ingram, M., Lofthouse, H. K., & Montagu, D. (2013). What is the role of informal healthcare providers in developing countries? A systematic review. PloS one, 8(2), e54978.